Valuable from didactical point of view
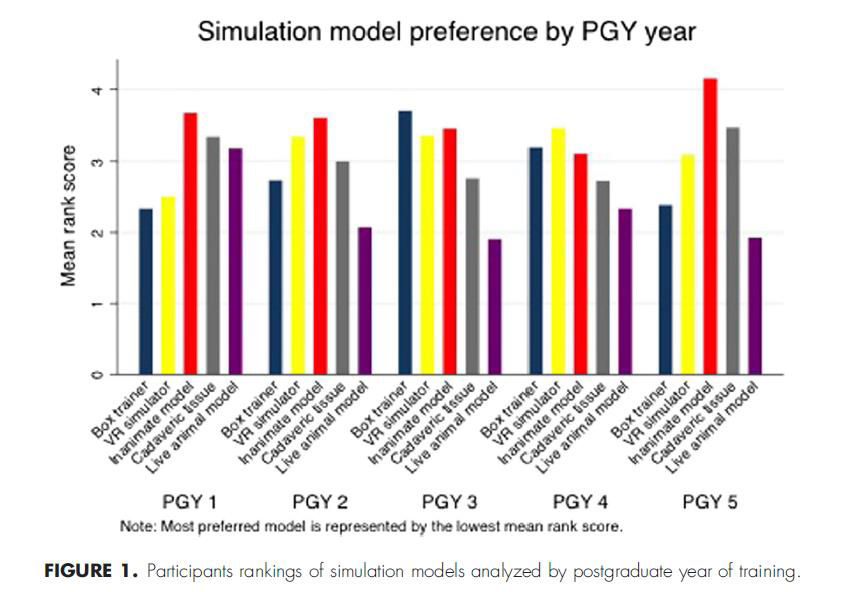
“A cross-sectional study on general surgery residents (postgraduate years 1-5) at Yale University School of Medicine and the University of Toronto via an online questionnaire was conducted. Overall, 67 residents completed the survey. Overall, 95.5% of the participants believed that simulation training improved their laparoscopic skills. Most respondents (92.5%) perceived that skills learned during simulation training were transferrable to the operating room. Overall, 56.7% of participants agreed that proficiency in a simulation curriculum should be mandatory before operating room experience.”
Shohan Shetty et al., “Perceptions, Training Experiences, and Preferences of Surgical Residents Toward Laparoscopic Simulation Training: A Resident Survey”, Journal of Surgical Education (in press)
Inanimate model appears to be the favorite of medical experts
Shohan Shetty et al., “Perceptions, Training Experiences, and Preferences of Surgical Residents Toward Laparoscopic Simulation Training: A Resident Survey”, Journal of Surgical Education (in press)
High adherence to real anatomy
“An on-line survey was developed. An email invitation to participate was sent to 600 members of the Canadian Orthopedic Association (it was not known if all of these surgeons performed arthroscopic surgery). A total of 111 orthopedic surgeons responded to the survey. These respondents performed an average of 185.3 procedures per year (SD = 132.4) and had on average 13.5 years of experience doing arthroscopy (SD = 8.3 years). Specifically, it was reported that identification and navigation skills were deemed to be the most important for a trainee to possess prior to entering the operating room. It was also suggested by the experts that very high fidelity simulation is preferred for training over low-fidelity bench top models.”
Safir et al. “What skills should simulation training in arthroscopy teach residents?”, Int J CARS, 2008
Greater skill improvement with simulators vs. cadavers
"Seventeen subjects applied to take part in the study. All subjects met the inclusion criteria, and none were excluded. Randomization resulted in 8 participants assigned to the VR group and 9 tonone were excluded. Randomization resulted in 8 participants assigned to the VR group and 9 to the BT group. Both simulators delivered improvements in arthroscopic skills. BT training led to skills that readily transferred to the VR simulator. Skills acquired after VR training did not transfer as readily to the BT simulator. Despite trainees receiving automated metric feedback from the VR simulator, the results suggest greater gain in psychomotor skills for BT training.”
Middleton et al., “Simulation-Based Training Platforms for Arthroscopy: A Randomized Comparison of Virtual Reality Learning to Benchtop Learning”, Arthroscopy: The Journal of Arthroscopic and Related Surgery (in press)
Future medicine admission tool (OR, univesities)
"Tools with the req-uisite levels of reliability and validity for summa-tive assessment include the OSATS and MISTELS programs. For example, the MISTELS program might be used to assess a resident's performanceof basic laparoscopic skills."
“A requisite level of performance would be required before the resi-dent would be allowed to perform a laparoscopic cholecystectomy. Similarly, OSATS stations could be used for open surgery. Residents would thus be trained in the laboratory until preset criteria had been met and would only then be allowed to participate in the graduated performance of pro-cedures in patients. Competence-based advance-ment, rather than time served, would become standard in surgical training.”
Richard K Reznik et al., “Teaching Surgical Skills - Changes in the wind”, the new England Journal of medicine, 2006
Cost effective- compared to other simulators and cadaver labs
“The disadvantages [of cadaver labs, ndr] are the costs, difficulty in procurement of cadavers, limits on repeated use of a cadaver, and the possibility of disease transmission.”
“Despite a general opinion that the more realistic the simulated experience, the better the trainees’ ultimate performance will be, no studies to date have demonstrated the superiority of haptic simulators over non haptic ones.”
Kivanc Atesok et. al, “Surgical Simulation in Orthopaedic Skills Training”, Journal of the American Academy of Orthopaedic Surgeons, 2012
“Most surgical training programs make use of a variety of models, including inanimate models, virtual reality, live animals, and human cadavers, to simulate living human tissue and anatomy, as well as high-performance patient simulators for critical-incident and team training. Although hu- man cadavers most closely approximate reality, their cost and limited availability, as well as the poor compliance of cadaveric tissue, limit their use. The use of live animals is also problematic because of ethical concerns, high costs, and the need for specialized facilities. In contrast, inani- mate models are safe, reproducible, portable, read- ily available, and generally more cost-effective than animals or cadavers.”
Richard K Reznik et al., “Teaching Surgical Skills - Changes in the wind”, the new England Journal of medicine, 2006
Physical models leads to faster and accurate arthroscopy
“A total of 23 subjects (17 novices and 6 experts) were recruited to participate in the study. The results show that the expert group completed the tasks more quickly than the novices, and that the novices completed the tasks more quickly after practice with the simulator. An analysis of the task completion time shows that experts completed the tasks more quickly than novices, and that, as expected, novices reduced their task time after practice. For the path length metric, experts completed the tasks using a shorter path, as expected, for all tasks. Novices decreased the path length from the pre-test to the post-test.”
McCracken et al., “Development of a physical shoulder simulator for the training of basic arthroscopic skills”, Int J Med Robotics Comput Assist Surg., 2017
“Subjects were recruited from among residents and attending surgeons in an orthopaedic surgery residency program. Each subject was tested on an arthroscopic shoulder simulator and objectively scored on the basis of the time taken to complete a standardized object selection program. After an interval of at least two weeks, each subject was then tested on a cadaveric shoulder arthroscopy model designed to replicate the shoulder arthroscopy simulator testing protocol, and the time to completion was again recorded. These results demonstrated a strong correlation between performance of basic arthroscopic tasks in a simulator model and performance of the same tasks in a cadaveric model.”
Martin et al., “Arthroscopic Basic Task Performance in Shoulder Simulator Model Correlates with Similar Task Performance in Cadavers”, J Bone Joint Surg Am., 2011
“Six fellowship-trained lower-limb surgeons were given standardized instruction regarding the performance of an arthroscopic Bankart suture on a laboratory-based simulator. They performed three single Bankart sutures on each of four occasions, one to two weeks apart. Six months later, the same surgeons repeated the study. This study objectively demonstrated a loss of all of the initial improvement in the performance of an arthroscopic Bankart suture following a six-month interval in which the surgeons did not do the procedure. The results indicate a need for regular repetition of some surgical tasks in order to maintain optimum performance levels and to consolidate the skills needed for newly learned procedures.”
Howells et al. “Retention of Arthroscopic Shoulder Skills Learned with Use of a Simulator”
Objective evaluation of surgeon skills on specific tasks
"A total of 23 subjects (17 novices and 6 experts) were recruited to participate in the study. The results from the task completion time and path length support construct validity for the simulator in terms of distinguishing between novices and experts and achieving the goal of helping novices improve through relevant practice."
McCracken et al, "Development of a physical shoulder simulator for the training of basic arthroscopic skills", Int J Med Robotics Comput Assist Surg., 2017
"We compared an experienced group of arthroscopic shoulder surgeons (Arthroscopy Association of North America faculty) (n=12) with a novice group (n=7) (postgraduate year 4 or 5 orthopaedic residents). The tool comprised by validated ABR metrics coupled with a dry shoulder model simulator is able to accurately distinguish between the performance of experienced and novice orthopaedic surgeons."
Angelo et al., “The Bankart Performance Metrics Combined With a Shoulder Model Simulator Create a Precise and Accurate Training Tool for Measuring Surgeon Skill”, Arthroscopy: The Journal of Arthroscopic and Related Surgery, 2015.
“Evaluating performance in the operating room is difficult,16 and most ef- forts have focused on techniques that standard- ize the assessment process outside the operating room. One such method is the Objective Struc- tured Assessment of Technical Skills (OSATS),17,18 in which candidates perform a series of standard- ized surgical tasks on inanimate models under the direct observation of an expert. Examiners score candidates using two methods. The first is a task- specific checklist consisting of 10 to 30 specific surgical maneuvers that have been deemed essen- tial elements of the procedure. The second is a global rating form, which includes five to eight surgical behaviors, such as respect for tissues, economy of motion, and appropriate use of assis- tants. The validity and reliability of the OSATS are similar to those of the more traditional Objective Structured Clinical Examination (OSCE) and are acceptable for summative high-stakes evaluation purposes.19-21 To date, we have created more than 40 OSATS stations; some examples are shown in Figure 1. Other methods of assessment include the Mc-Gill Inanimate System for Training and Evalua- tion of Laparoscopic Skills (MISTELS)22 and the Imperial College Surgical Assessment Device (ICSAD).23,24 Developed at McGill University in Montreal, the MISTELS uses an inanimate box to simulate the generic skills needed in the perfor- mance of laparoscopic surgery. It has been shown to be a valid and reliable instrument for assess- ing laparoscopic skills.22 The ICSAD, developed at Imperial College in London, tracks hand motion using sensors placed on the trainee’s hands during the performance of a task. The sensors translate movement into a computerized tracing of hand motion, which provides an effective index of tech- nical skill in both laparoscopic23 and open24,25 procedures. This index has been shown to have good concordance with OSATS scores.”
